CHF Mortality Benefits: Pump Up the Volume
/Scenario 1:
Chief Complaint: 32 year old non-pregnant female, non-smoker, occasional alcohol use, no significant past medical history presenting with dyspnea and reports of lower extremity edema. I give you the following tools:
- Physical exam
- CXR
- EKG
- Pro-BNP
- Framingham Heart Failure Diagnostic Criteria
- You don't get to choose an echocardiogram (too easy)
Which ones do you want to use for your evaluation if you're at all concerned about CHF (which you're probably not), specifically systolic CHF (HFrEF)?
Scenario 2:
Chief Complaint: 57 year old male, 30 pack year smoker, moderate alcohol use, past medical history significant for hypertension, diabetes and hyperlipidemia presenting with dyspnea and reports of lower extremity edema. I give you the following tools:
- Physical exam
- CXR
- EKG
- Pro-BNP
- Framingham Heart Failure Diagnostic Criteria
- You don't get to choose an echocardiogram (too easy)
Which ones do you want to use for your evaluation if you're at all concerned about CHF? (which you probably are)
Best Practice Answer:
Scenario 1: Framingham Heart Failure Diagnostic Criteria, Pro-BNP, and maybe an EKG
Scenario 2: Physical exam and CXR
I'm willing to bet those weren't your selections for each one.
I recently gave a talk on outpatient CHF management and the answer to these scenarios surprised me. I have thought for many years now that the CXR was something that docs ordered blindly without reason in suspected CHF cases. Now that may still be the case but at least they have some good data to back them up. At the same time, Pro-BNPs are becoming more and more of a regular occurrence in diagnostic work ups and they're really best suited for only one side of the CHF equation.
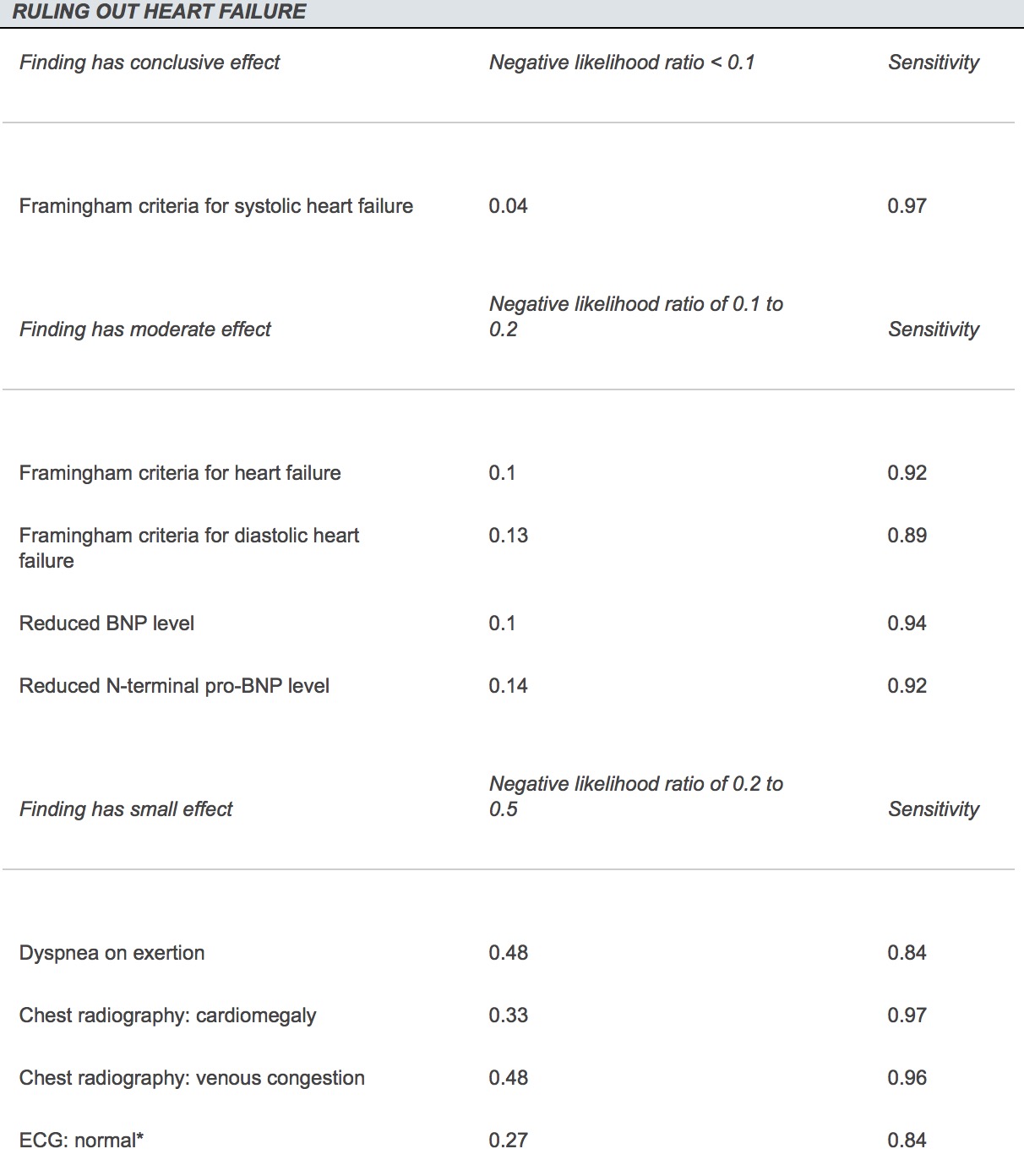
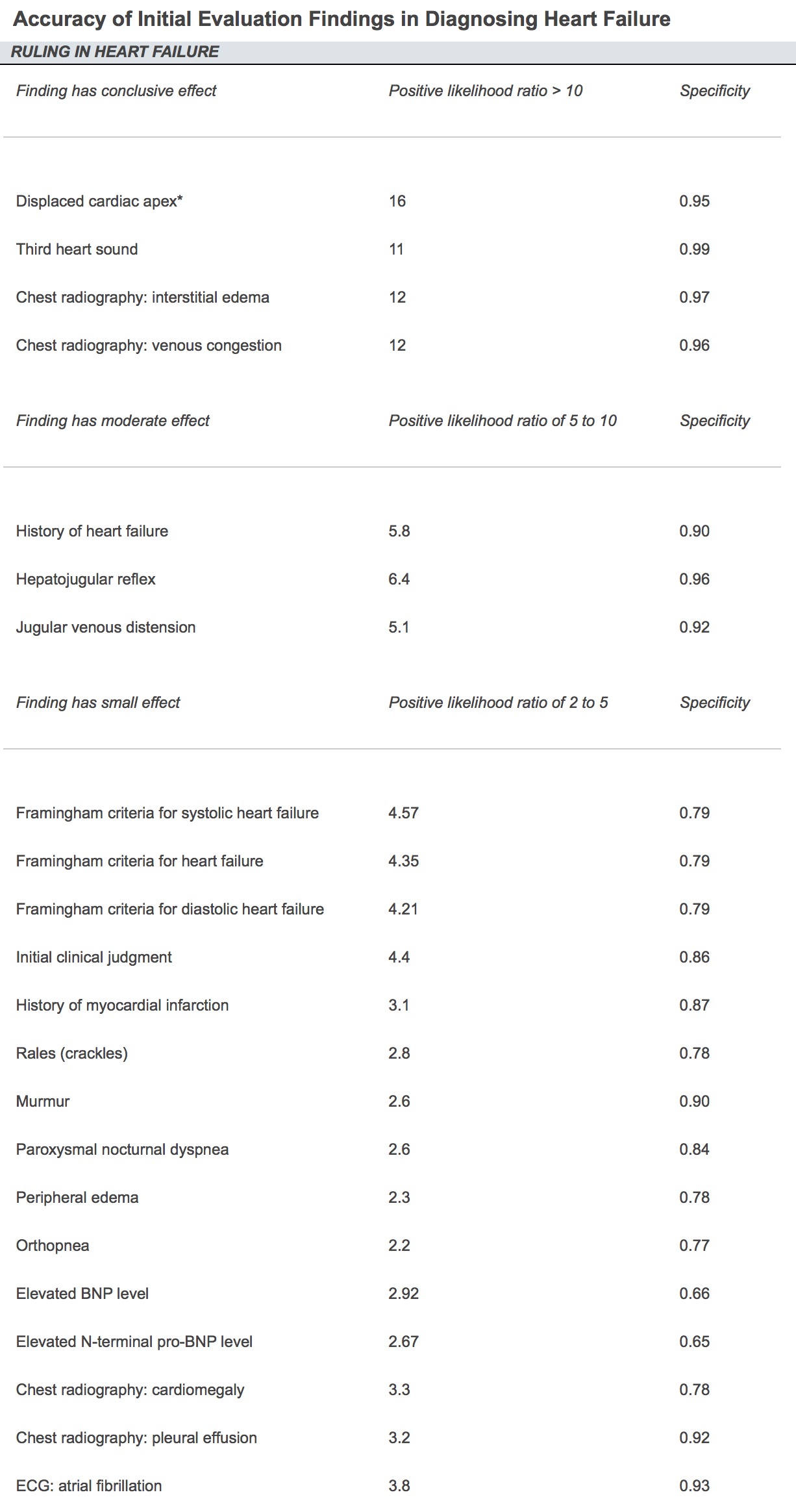
Taking a look at the likelihood ratios compiled below from a 2012 AFP article we can see that the strategy for ruling IN CHF is not the same as ruling OUT CHF.
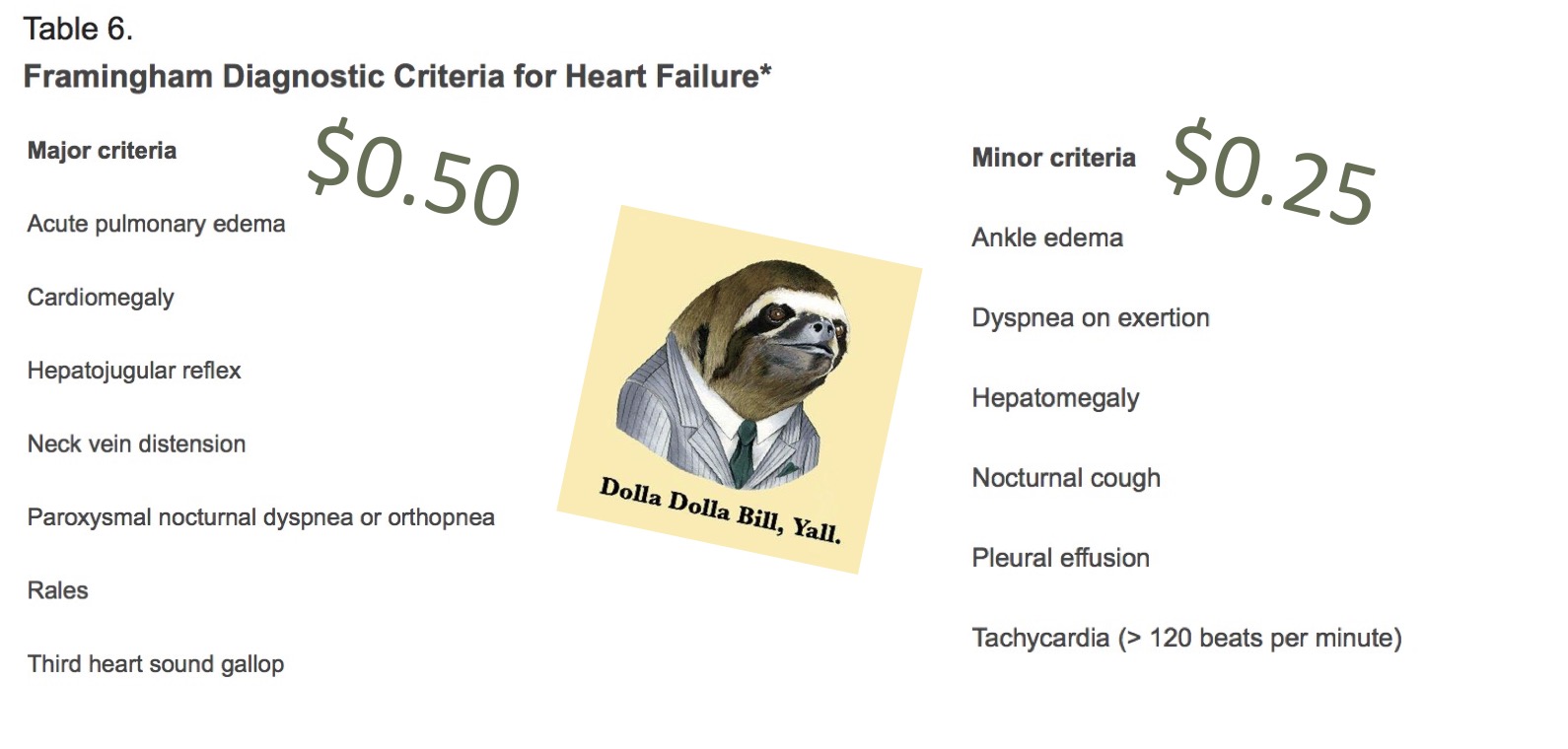
The healthy 32 year old female has a low pre-test probably of having CHF because of the low prevalence in her specific cohort (young and healthy). Remember that prevalence affects likelihood ratios. We're going to want to use strategies with low negative likelihood ratio (-LR) to rule out the small chance she has CHF. As you can see above, the Framingham criteria for heart failure (especially systolic heart failure) as well as a reduced Pro-BNP level (typically < 300) have a low -LR and would be great tests to use in this case. Hard time remembering how to make a diagnosis with the Framingham criteria? Just remember that if you can make $1 between the two lists you have a diagnosis (see below). One final thing I would add is that EKG's are excellent at ruling out systolic heart failure if normal (98% NPV). [1] Just don't rely on them to rule anything in or rule out diastolic heart failure.
Now what about scenario 2? Use the opposite logic. A patient who has a HIGH pre-test probability of CHF (smoker, hyperlipidemia, older) can more accurately be ruled IN for the diagnosis with a higher positive likelihood ratio (+LR). So in this case I would reach for some rather easy physical exam findings (S3, displaced cardiac apex) and the aforementioned CXR. Remember though that the findings you're looking for are interstitial edema (Kerley B lines) and pulmonary edema. As you can see further down the list, cardiomegaly and pleural effusion don't help you as much.
An interesting side note is how low many of the signs and symptoms we normally report are in the list. Crackles, peripheral edema, PND and orthopnea are all rather low on the list for +LR.
What Saves Lives in Systolic Heart Failure?
Flavor 1: ACE Inhibitors
Flavor 2: Beta-blockers
ACE inhibitors and beta blockers share lots of similarities. They both have a substantial amount of old but credible data to back them up. They both have been found to improve function (NYHA classification) in patients with systolic heart failure (HFrEF) . They both show improvement in all-cause mortality. [2,3,4] You should use both of these any chance you get in your HFrEF patients. Long term outcomes aren't affected by which one you start first but some would argue to start the ACE inhibitor first due to beta blockers potentially causing further acute decompensation.
Flavor 3: Mineralcorticoid Receptor Antagonists (Spironolactone)
Once your patient is already titrated up on the above medications you should begin thinking about additional therapies if their function isn't optimized (NYHA 2-4). MRA's have been shown to improve all-cause mortality, hospitalization rates, and function status in those already on medical therapy. You want to remember to check the potassium since it's potassium sparing. American Heart Association (AHA) has the unrealistic monitoring schedule recommendation of 2-3 days after starting therapy, 1 week after, then monthly for 3 months then every 3 months after that. Just food for thought.
Flavor 4: ARNI's
Angiotensin Receptor-Neprilysin Inhibitors. Mouthful. These guys are a combo drug with Sacubitril and Valsartan. You already know what Valsartan does. Sacubitril is the Neprilysin inhibitor. What is Neprilysin? It's an endopeptidase that cleaves vasoactive peptides such as BNP. The rationale is to inhibit the inhibitor to ensure a healthy amount of BNP is floating around to vasodilate. Newer RCTs have found a reduction in all-cause mortality and hospitalization rates BEYOND ACE inhibitors. [5] The indications can be somewhat narrow though. Recommendations are to consider ARNI's if the following criteria are met:
- LVEF < 40%
- Elevated BNP or heart failure hospitalization in past year
- SBP > 100
- GFR > 30
- Those who have tolerated ACE inhibitor in the past
If that sounds like one of your patients this might be a consideration but just remember that ACE inhibitors have years of good data showing improvement in patient centered outcomes while ARNI's haven't had quite that amount of data to back it up.
Flavor 5: Cardiac Devices
I won't go into too much detail here as placing ICDs and CRTs don't quite fit my scope of practice. But it's important to remember that cardiac devices have been shown to improve outcomes in certain subgroups of patients. Specifically, they have been shown to improve all-cause mortality compared to medical therapy [6]. These results have ranged anywhere between 28-53% improvement based on which type of device was studied. CRT-D was found to have the largest mortality benefit. What is CRT-D vs CRT-P vs ICD? Good question since I didn't know the difference myself beforehand. Here's the breakdown:
- ICD: Lead in right atrium and right ventricle. Used to shock abnormal rhythms.
- CRT-D: Lead in right atrium, right ventricle and left ventricle to help synchronize the pumping of blood to the rest of the body. These include an ICD as well.
- CRT-P: Same as the CRT-D except without the ICD.
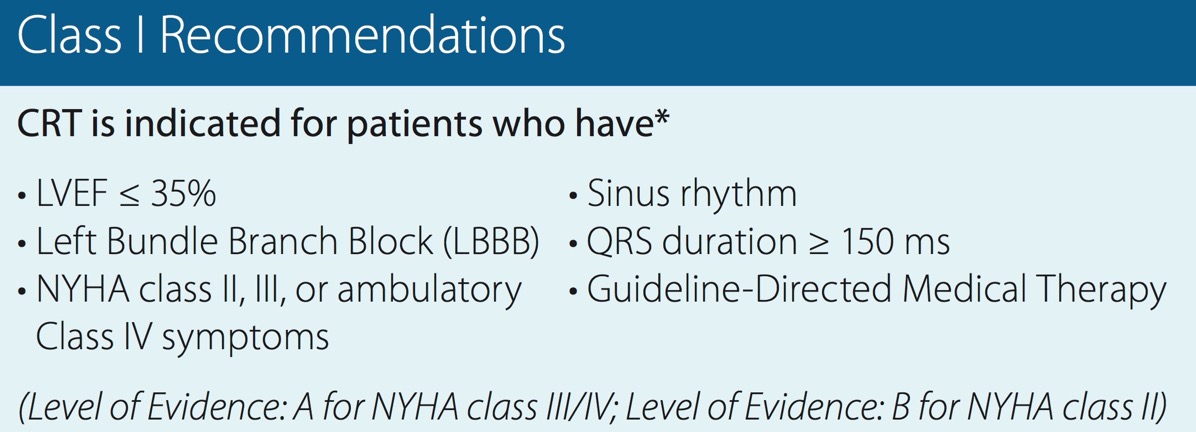
What patients receive the most benefit? The 2012 AHA recommendations are divided by classification of recommendations (1-3) and level of evidence (A-C). Here are the Class 1, Level A recommendations:
Quick Shout Out
I didn't discuss treatment modalities that improve morbidity but there are a number of these as well for systolic heart failure. These include digoxin, immunizations (flu, pneumococcal), diuretics, and cardiac rehabilitation. There was subgroup analysis from the DIG trial previously that did show some mortality benefit for digoxin when those patients were within the 0.5-0.8 ng/mL range for serum digoxin concentration. The downside is that when this level increased above 1.2 there was actually an increase in mortality rates. It's also just a tricky medication to use overall that requires close monitoring.
You Forgot Diastolic Heart Failure (HFpEF)!
You're right. I didn't mention diastolic heart failure since there is no substantial evidence to show any mortality benefit in any specific treatment option. Exercise training is the only intervention to show improvement in quality of life and exercise capacity [7]. Unfortunately neither Medicare or Medicaid cover this for diastolic heart failure. So we're stuck with symptom management and contributing factor management for treatment.
So remember next time you want to rule IN someone with a high likelihood of CHF go for the CXR and cardiac exam. If you want to rule OUT someone with a low likelihood of CHF go for the Pro-BNP, Framingham Heart Failure Criteria, and potentially an EKG. Once you make that diagnosis you can reach for your five lifesaver flavors to help improve mortality rates for your patients.
Quick plug for my new podcast Greyscale. It can be found on iTunes or anywhere you like to get your podcasts. Two episodes currently up with a third on the way. I'll also be launching a Sports Medicine Podcast (The Break) in the near future as well!